But what makes them different from the original strain? The following visualizations answer some key questions, including when these variants were first discovered, how far they’ve spread worldwide, and most importantly, their potential impact on the population.
Some Context: What is a Variant?
Before diving in, it’s important to understand why viruses mutate in the first place. To infect someone, a virus takes over a host cell and uses it to replicate itself. But nature isn’t perfect, and sometimes, mistakes are made during the replication process—those mistakes are called mutations. A virus with one or more mutations is referred to as a variant. Most of the time, variants do not affect a virus’s physical structure, and in those instances, they eventually disappear. However, there are certain cases when a mutation impacts part of a virus’s genetic makeup that does change its behavior. According to the U.S. Centers for Disease Control (CDC) a change in behavior can alter:
Rate of transmission Deadliness Ability to potentially infect someone with natural or vaccine-induced immunity
Preliminary research has detected some of these changes in the three major COVID-19 variants—B.1.1.7, B.1.351, and P.1.
The 3 Major COVID-19 Variants
The three major variants emerged at different times, and in different parts of the world. Here’s an overview of each variant, when they were discovered, and how far they’ve spread so far.
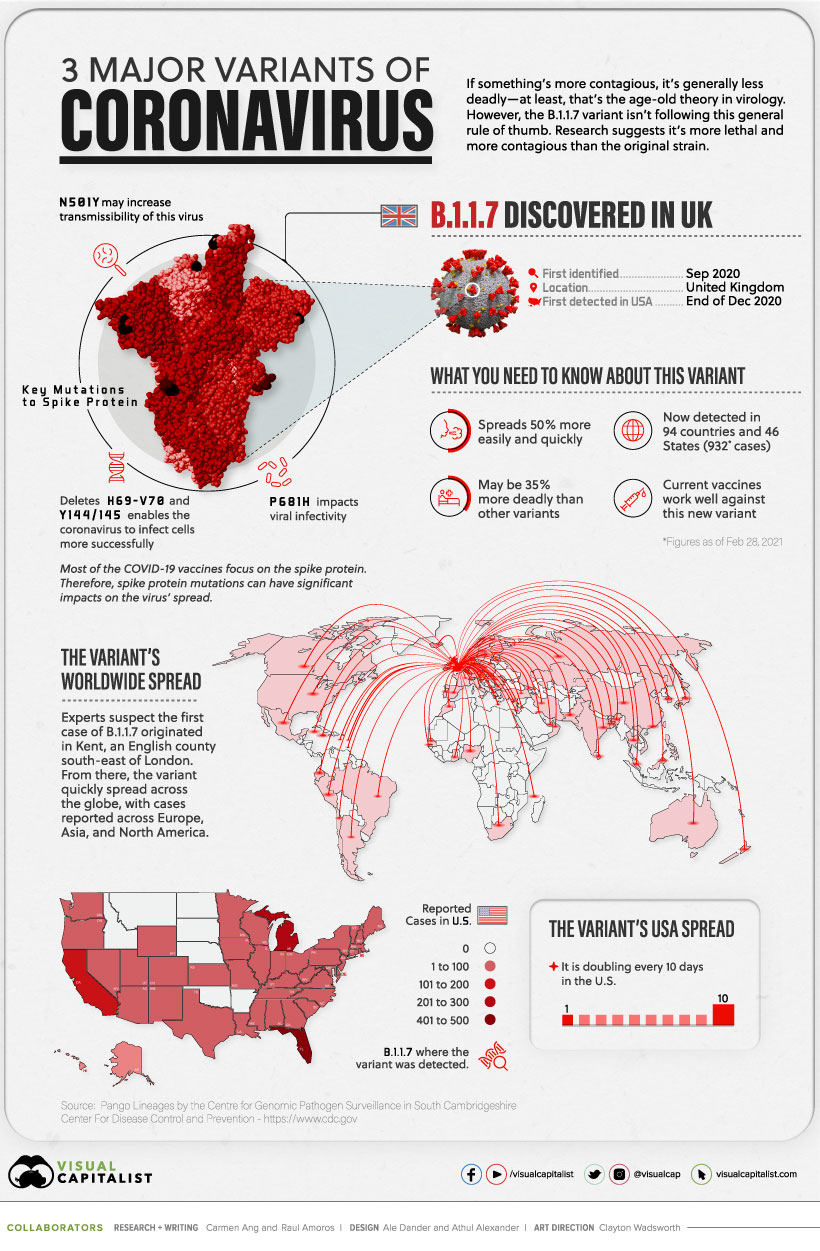
B.1.1.7
The B.1.1.7 variant was detected in the UK in the fall of 2020. By December 2020, it had spread across the globe, with cases emerging across Europe, North America, and Asia.
Currently, the variant has been reported in roughly 94 countries. Early research suggests it’s 50% more transmissible than other variants, and potentially 35% more deadly than the standard virus. Luckily, studies suggest that some of the existing vaccines work well against it.
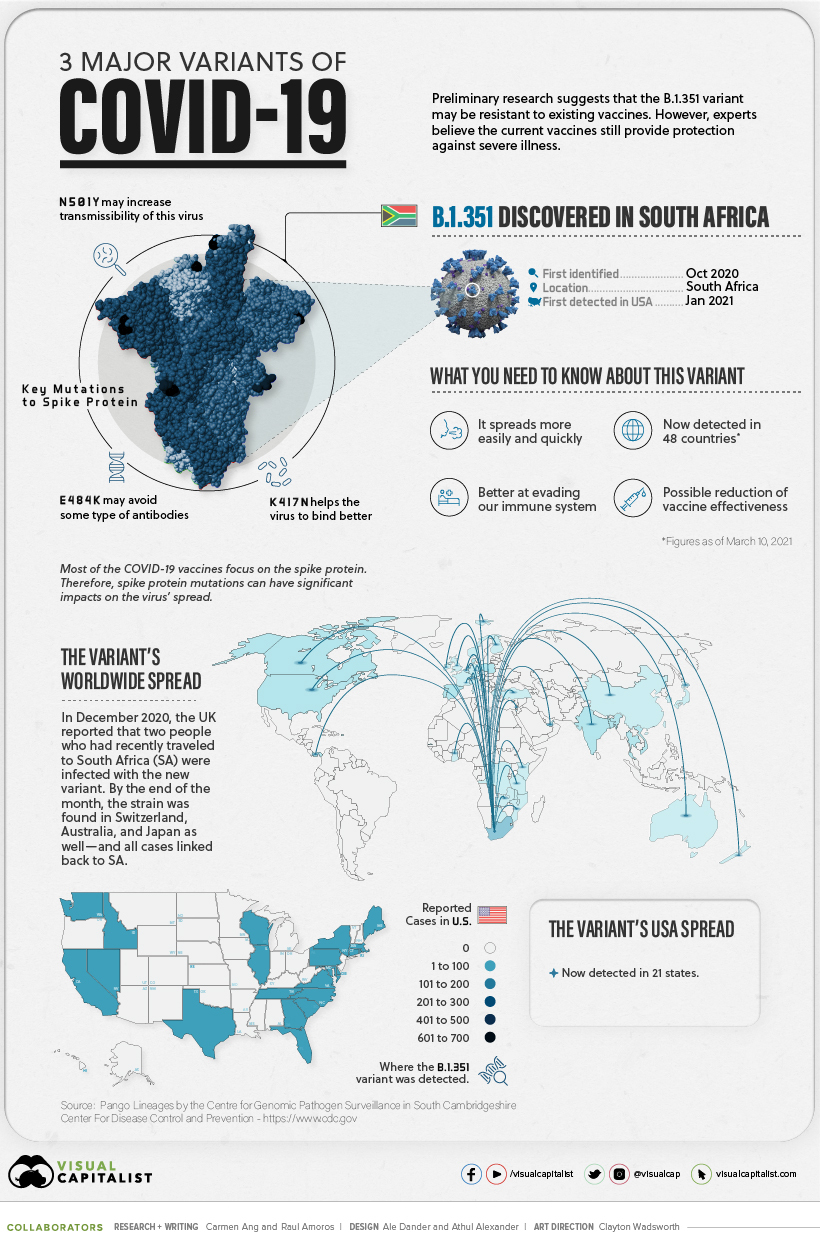
B.1.351
In October 2020, the second major variant was discovered—B.1.351. It was first identified in South Africa, but by end of the year, it had spread to the UK, Switzerland, Australia, and Japan.
There are approximately 48 countries with reported cases, and research suggests several of the existing COVID-19 vaccines may not be as effective against this variant.
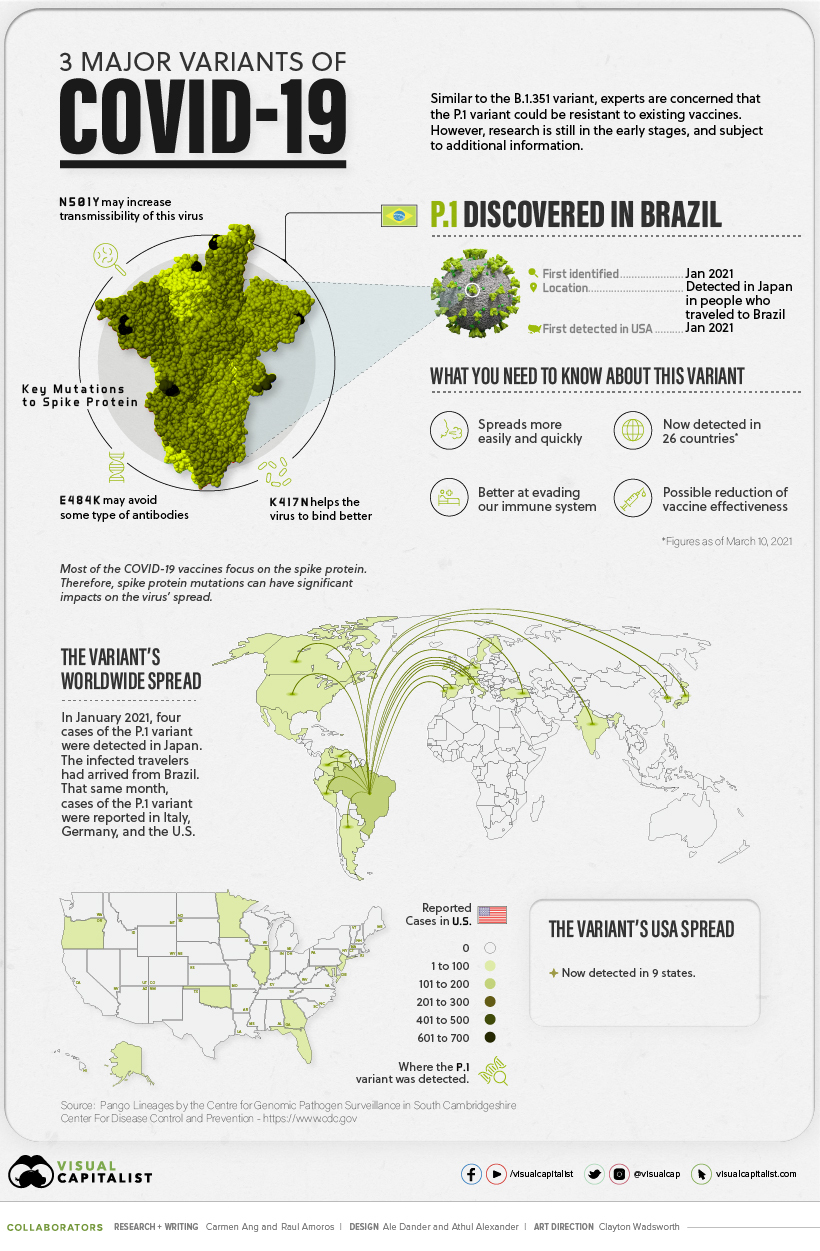
P.1
The P.1 variant was the last to arrive on the scene. It was first discovered in January 2021, when Japan reported four cases of the variant, which was found in travelers who had arrived from Brazil.
Approximately 25 countries have reported cases of the P.1 variant, and early research suggests this variant is not only more contagious, but could also have the ability to infect people with natural immunity who had already recovered from the original strain.
Still Early Days
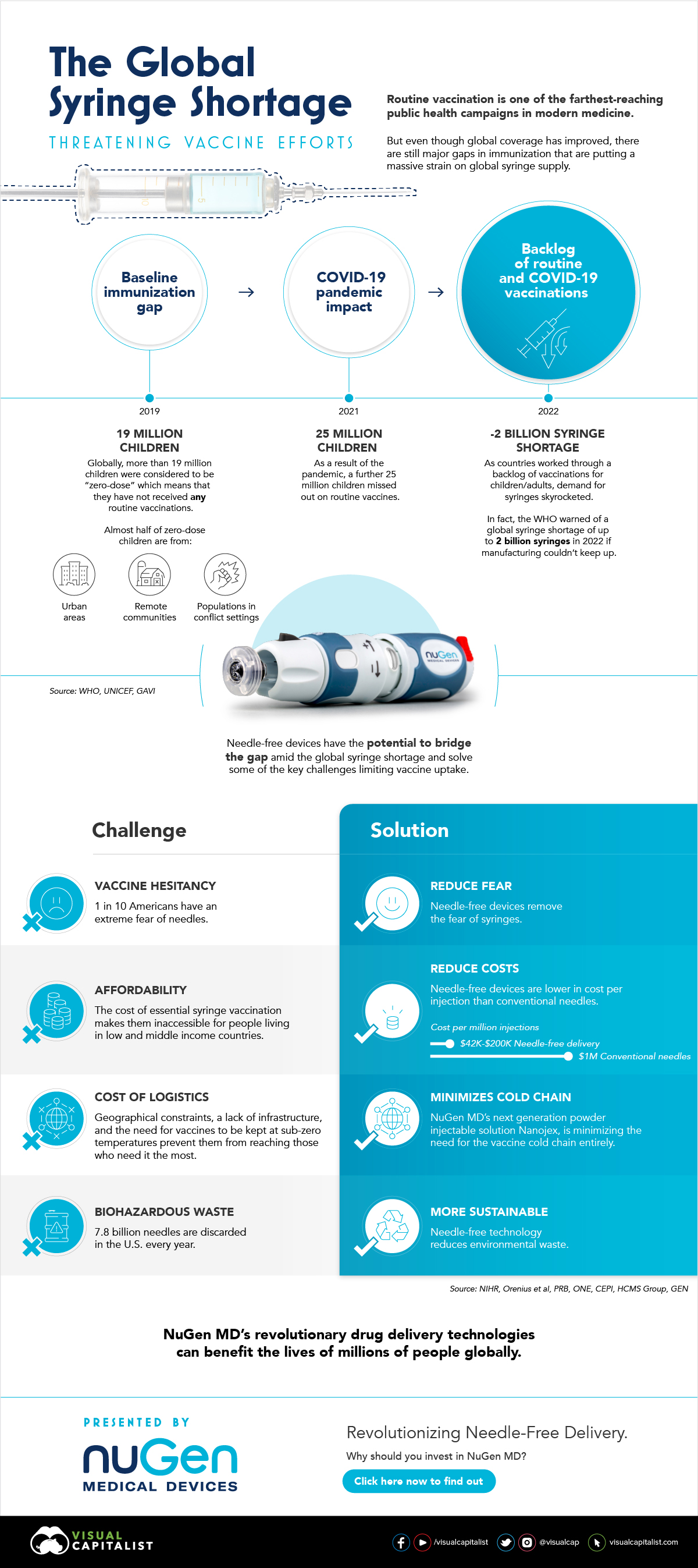
While there have been preliminary studies showing a dip in vaccine effectiveness, some experts emphasize that it’s too early to tell for certain. More data is needed to gain a deeper and more accurate understanding. In the meantime, experts are emphasizing the importance of following our current public health strategies, which include physical distancing, vaccination, washing your hands, and using masks. on In the above infographic from NuGen Medical Devices, we explore the factors leading to the syringe shortage and take a look at the company’s innovative needle-free solution that could play an important role in closing the immunization gap.
The Immunization Gap
Even before the COVID-19 pandemic, millions of people around the world struggled to get access to routine vaccinations. In fact, as of 2019 more than 19 million children around the world were considered to be “zero-dose” which means that they did not receive any routine vaccinations. Moreover, when the COVID-19 pandemic hit, global immunization dropped even further with 25 million children missing out on routine vaccines in 2021 alone.
Why is Immunization So Important?
Vaccinations prevent against over 20 life-threatening diseases and save between 2-3 million deaths per year, making them—as the WHO describes—the foundation of healthcare systems and an indisputable human right. As countries work through a backlog of vaccinations to close the immunization gap that has worsened since the pandemic, demand for syringes has significantly increased.
The Result: A Global Syringe Deficit
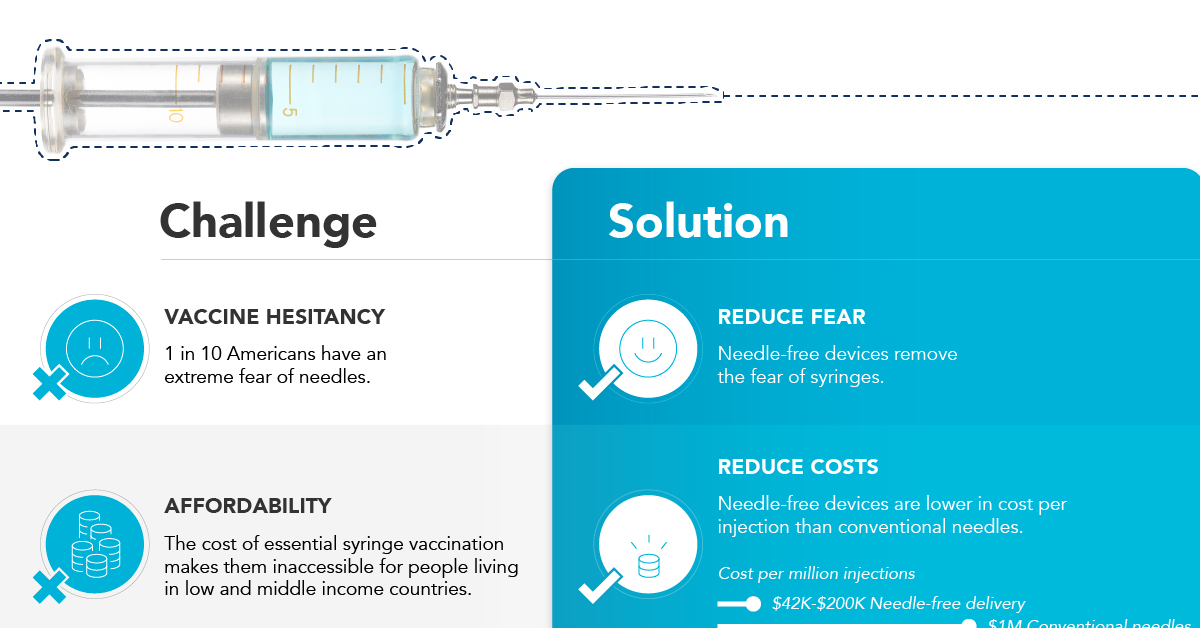
In 2022, the WHO warned that we could see a shortage of up to 2 billion syringes if manufacturing can’t keep up. This could result in the severe disruption to routine vaccinations and promote unsafe recycling of syringes in order to administer vaccines. But the issue goes far beyond a supply shortage of syringes. COVID-19 has brought conventional syringe vaccines into sharp focus, with many criticizing the challenges associated with them. With conventional needles facing so many challenges, it’s no surprise that investors are taking interest in viable alternatives. What’s more, these alternatives don’t just apply to vaccinations, they can also work for people with diabetes, dentists, and pet care.
Enter Needle-free Devices from NuGen MD
Needle-free devices have the potential to bridge the gap in immunization amid the global syringe shortage, solve some of the key challenges limiting vaccine uptake, and more importantly, benefit the lives of millions of people.
How Do They Work?
NuGen’s needle-free devices use a simple spring-loaded mechanism which uses pressure to release the liquid drug and penetrate the skin. In less than one-tenth of a second, the drug is dispensed more safely and evenly compared to needle syringes. It’s also virtually painless and leaves no mark on the skin.
Interested in investing in NuGen Medical Devices? To learn more about their plans to pioneer the future of needle-free drug delivery, click this link now.